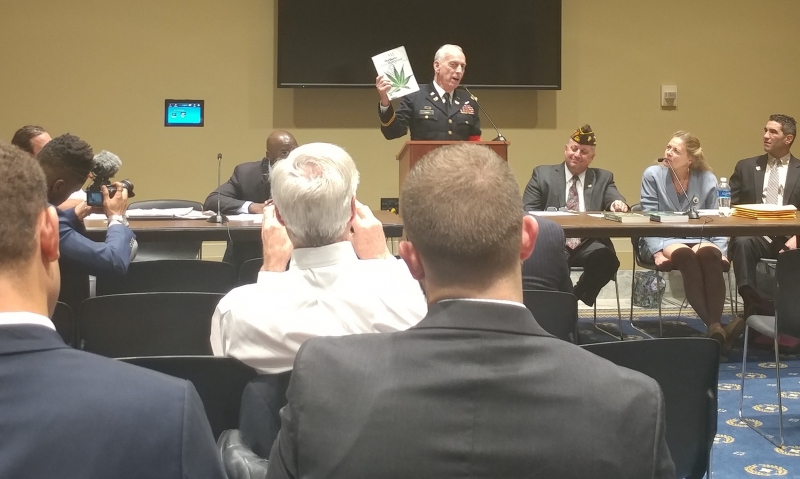
Health care professionals and former servicemembers discuss what medical cannabis could look like for veterans.
Hoosier Veterans for Medical Cannabis Inc., in cooperation with the Congressional Cannabis Caucus, hosted a forum Sept. 13 to convene with health care professionals and former servicemembers to discuss what medical cannabis could look like for veterans. More than 25 guests attended the forum, held inside the Gold Room of the Rayburn House Office Building in Washington, D.C.
Dr. Jordan Tishler, a Harvard Medical School graduate and advocate for marijuana regulation and product development, was one of the first panelists to speak. Over the last 15 years, Tishler said he’s treated numerous veterans who have been harmed by substances like alcohol, medications and opioids.
“One of the things we need to understand is that pain is the number one complaint across America,” he said. “It’s the number one complaint that patients report back to us that we’re not doing a good job taking care of.”
When it comes to treating pain, Tishler said the problem is people simply don’t have a lot of choices. Opioids, for example, aren’t super effective for treating chronic illnesses.
“What we know is that roughly 68,000 veterans are primarily dependent upon opioids,” he said. “Thirty-five percent of veterans misuse, in some fashion or another, the opioids that they’ve been given.”
Tishler said medical cannabis, when combined with the use of opioids, is a safer alternative for treating chronic illness. Studies have shown that cannabis is not only more effective, but also lessens one’s chances of dying.
“The other thing that we need to recognize is that mental illness and PTSD interacts bi-directionally with chronic pain and opioid misuse,” Tishler said. “What this means is that opioid use and chronic pain influence mental health, and mental health worsens people’s pain and abuse of opioids.”
According to Tishler, studies have shown that cannabis use is not associated with increases in violent behavior or change in socioeconomic health costs. In addition, states with medical cannabis laws have nearly seen a 25 percent reduction in overdoses from opioid use; 23 percent reduction in hospitalizations related to opioid abuse; and 13 percent reduction in hospitalizations related to complications of opioid medication use.
“If you treat somebody with cannabis as well as opioids, you end up needing only about 20 percent of opioid which reduces their risk of death. So, using these together is an effective combination,” Tishler said. “We see about a 7 to 9 percent dependence rate and people get very concerned about that. But let’s also remember that means 91 to 93 percent of people don’t have any issue at all. For comparison, we need to look at (benzodiazepines), like ativan and valium – that dependence rate is 18 percent. The opioid rate is up to 25 percent making cannabis, again, look pretty good.”
A research paper presented in 2013 at an international drug policy symposium in Auckland, New Zealand, backs Tishler’s thoughts on reduced dependency and concluded that nine out of 10 regular cannabis users do not become dependent on the drug. The paper specifically noted that, “the lifetime risk of developing dependence among those who have ever used cannabis was estimated at 9 percent in the United States in the early 1990s as against 32 percent for nicotine, 23 percent for heroin, 17 percent for cocaine, 15 percent for alcohol and 11 percent for stimulants.”
Over the past few years, many veterans have come forward to tell The American Legion leadership that access to cannabis has improved their quality of life. The American Legion has been advocating for research into alternative treatments for post-traumatic stress disorder and traumatic brain injuries, and passed Resolution 28 during its 99th National Convention last month in Reno, Nev. The resolution calls for permitting VA medical providers to openly discuss with veterans the use of marijuana for medical purposes, as well as recommend it where legal.
Veterans for Medical Cannabis Access Executive Director Michael Krawitz, an Air Force veteran, mentioned that he made an amazing discovery about cannabis in the mid-1990s after years of suffering long term and chronic pain.
“It was on a trip abroad that I was first prescribed cannabis as an adjunct to my pain treatment,” Krawitz wrote for the American Medical Association Journal of Ethics in 2015. “I found that, with cannabis, I was able to use an amount of opiates small enough to reduce side effects while allowing me to function better than I did when taking the higher dose.”
Dr. Ziva Cooper, an associate professor of clinical neurobiology in the Department of Psychiatry at Columbia University Medical Center, studies the direct effects of cannabis and cannabinoids in volunteers. She said people who use medical cannabis are not doing so to have fun or get high, rather they use it because they want symptom relief.
“Cannabis Use Disorder (CUD) is defined as the continued use of cannabis despite clinically significant distress or impairment,” she said. “The prevalence of lifetime diagnosis of CUD is 6.3 percent, and 1-in-3 heavy cannabis users.”
Cooper suggested that the more people smoke cannabis, the more likely they are to develop CUD. But this is an important part of discussion of the utility of medical cannabis, and the importance of future research on how to harness its therapeutic effects while diminishing its adverse effects, she said.
“We found moderate evidence for an association between PTSD symptom severity and Cannabis Use Disorder, but it is important to note that we could not come to a conclusion regarding the direction of this effect,” Cooper said. “Based on self-report and survey data, PTSD is one of the primary reasons people seek out medical cannabis and, importantly, people report that it provides symptom relief, suggesting that people are using cannabis and benefiting.
“Though we have yet to establish the therapeutic efficiency of cannabis or cannabinoids for PTSD, preclinical findings are very encouraging, pointing to the protective effects both THC, the primary psychoactive component of cannabis, and CBD, another non-intoxicating component of cannabis in (our testing).”
Furthermore, Cooper said there are enormous gaps in the knowledge. Because of this, there is also a desperate need for high quality studies to determine how the strong preclinical studies extend to a clinical population.
“We are in the midst of significant changes, people are utilizing cannabis-based products for medicine in over half of the United States,” she said. “It is our duty to address this significant public health issue and embark on rigorous study of both the therapeutic and adverse effects of cannabis and cannabinoids. It is only with these studies that the medical community, public health officials and leaders of our nation will be able to provide sound, data-driven information regarding how to approach the use of cannabis based products as medicine.”
Jeff Staker, founder of Hoosier Veterans for Medical Cannabis who organized the forum, addressed the concerns of veteran deaths due to overdoses and suicide since 9/11.
“We’ve got 22 veterans passing away every day and taking their own lives,” he said. “We shouldn’t deter from cannabis being a medicine like it’s supposed to be and can be. We don’t have a choice but to fight. That’s the way I look at this campaign. I treat it just like a military operation – if we don’t do nothing, more guys are going to die.”
Dr. Darryl Hudson, Canadian cannabis plant scientist and research project consultant, has studied the effects of different cannabis varieties for PTSD, which has lead to breeding new varieties designed specifically to alleviate the symptoms of PTSD.
“There is not a single country out there that actually supports the use of medical cannabis for veterans. But we’re changing that paradigm and we’re changing it drastically as we see results,” he said. “We’ve had six suicides in our program. Out of thousands of patients, all six were without cannabis medication at the time. Cannabis is the most effective drug on the planet that we’ve ever identified for treating PTSD.”
For Marine Corps veteran Ryan Miller, co-founder of Operation Educating Veterans About Cannabis, medical cannabis is a great alternative for veterans. He said it is not only less threatening to one’s health, but also alleviates symptoms associated with combat PTSD and can be a great resource for helping veterans find jobs in the cannabis industry.
“Even though cannabis is the best treatment, it is not a cure for PTSD,” Hudson added. “The government spends billions on drugs the first two years that a veteran comes home. If they spend even a fraction of that growing quality medicine for these guys, it would save lives. It would save money.”
Cooper said it is abundantly clear that veterans nationwide are turning to cannabis for help as 41 percent of them use it for medical purposes.
“That is over two times the rate of cannabis users in the general population,” she said. “It is critical that we understand the therapeutic potential of cannabis, cannabis-based products and cannabinoids in this population.”
- Veterans Healthcare

